Researchers find they can take somatic skin cells from pigs, program them into iPSCs and then inject them back into the same animal to treat the disease.
September 20, 2022
A new approach is paving the way for improved stem cell therapies and regenerative applications using cells from pigs. Led by Wan-Ju Li, a SCRMC researcher and associate professor in the Department of Orthopedics and Rehabilitation and the Department of Biomedical Engineering, this new study published in Scientific Reports offers a viable strategy to enhance the generation of induced pluripotent stem cells from large animal cells and provides researchers with insight into the underlying mechanism controlling the reprogramming efficiency of cells. In turn, this approach will allow researchers to reprogram cells more efficiently into iPSCs which can be used to study regenerative therapies aimed at treating everything from osteoarthritis to heart disease.
While this approach can be applied to regenerative therapies targeting any organ or tissue, Li and his Musculoskeletal Biology and Regenerative Medicine Laboratory study cartilage, so he developed the model by deriving iPSCs from the fibroblast cells of three different breeds of miniature pigs including Wisconsin miniature swine, Yucatan miniature swine and Göttingen minipigs. Fibroblast cells are easily obtained for cellular reprogramming and Li is interested in using these cells to efficiently develop cartilage cells that can be used to help patients experiencing osteoarthritis. But, while his goal for the study was specific, the model has wide-reaching implications.
"This model we created can be used for many applications," says Li. "In successfully developing iPSCs from three different breeds of minipigs, we learned we can take somatic skin cells from these pigs that we programmed ourselves into iPSCs and then inject them back into the same animal to treat the disease. Or we can take the cell that carried the disease gene and put that into the culture dish and use that as a disease model to study disease formation."
Li explained that iPSCs can be created from nearly any type of somatic cell, such as skin or blood cells, that are reprogrammed back into an embryonic-like pluripotent cells. These pluripotent stem cells are the body’s master cells and are, therefore, able to become nearly any cell in the body. Harnessing the power of such a cell and being able to grow these versatile cells in the lab is invaluable to medicine as these cells can be used for the regeneration or repair of damaged tissue and in drug testing to see how medication will impact heart, liver, or other cells within the body.
Through this research, Li and his lab have provided researchers with insight into the underlying mechanism controlling the reprogramming efficiency of iPSCs, allowing researchers to harness to power of iPSCs and develop them more efficiently. Specifically, he discovered that the expression level of the switch/sucrose nonfermentable component BAF60A, which is essentially a protein that can remodel the way DNA is packaged, helps to determine the efficiency of iPSC generation. He also noted that the BAF60A is regulated by STAT3, a transcription factor protein that plays a role in cell growth and death. Through this, Li discovered that the efficiency of iPSC generation is based on the expression level of these proteins and that the expression levels vary among pig breeds.
"While we successfully developed iPSCs and programmed iPSCs from the three different strains of pig, we noticed that some pigs had a higher reprogramming efficiency," says Li. "So, the second part of our findings, which is significant in biology, is understanding how these differences occur and why."
Li shared that understanding why different pig breeds have varying levels of reprogramming efficiency will directly translate to understanding differences in the effectiveness of iPSC generation between individual humans. In fact, a previous study by Mackey et al., has shown that a person's ethnicity may impact their cell's reprogramming efficiency. So, understanding what mechanisms control cellular reprogramming will be crucial to developing effective protocols of iPSC generation for individualized therapies.
"With this model, we can study musculoskeletal regeneration particularly cartilage regeneration for osteoarthritis patient," says Li. "But we think the impact is way beyond the application of orthopedics because from now on, anybody on campus who is interested in using the technology we have developed for a minipig model, can reprogram their cells into iPSCs and then these cells and the animal can be used to investigate heart disease, kidney disease, neuronal disease or any type of a disease."
Translating this research to improve human health, is deeply important to Li. He has spent much of his career studying novel approaches to regenerate cartilage and bone for orthopedic applications and developing a translational model like this means that science is one step closer to healing more patients using stem cells.
"I feel really touched by the stories people share. You cannot imagine how many emails come in asking me if they can become the first human patient in our future clinical trial," Li says. "People are in desperate need for something, especially when those people feel the current surgical procedure or intervention is not suitable for them. I have to keep saying, 'wait for another two, three years, maybe we'll be ready for a clinical trial,' but for me, it's time to move on and really do our larger animal studies to fulfill our promise. At least that way, I can fill the gap between the lab and clinical trials as the larger animals must be studied before you go into a clinical trial."
Li's development of a reliable and translational model for the generation of iPSCs in a large animal is critical as it has been a challenge to generate pig iPSCs with efficiency. The reprogramming efficiency of pig cells is relatively low compared to that of human or mouse cells, but large animal studies remain a crucial step in bringing treatments to clinical trials.
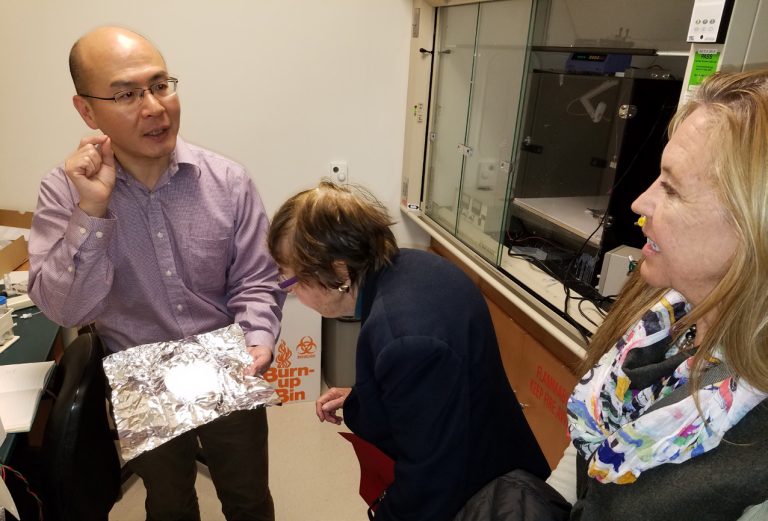
Interest in moving these treatments forward has grown and while this study was funded in part by NIH, Li also received support from the Plunkett Family Foundation in Milwaukee through their donation to the UW Stem Cell and Regenerative Medicine Center. After hearing of Li's research, Gwen Plunkett and her daughter Karen visited Li and his lab in 2019 to learn more and were inspired to support research into stem cells for cartilage regeneration.
"Innovation in medicine sparks critical change, for the world and the survival of our species – and the Plunkett Family mission is to be a catalyst in stem cell and regenerative medicine research," says Karen Plunkett. "We supported Jamie Thomson's lab in the early days when federal funding for human stem cell research was restricted. More recently, we continued our commitment to this research by supporting Dr. Wan-Ju Li's stem-cell based approaches for regenerating skeletal tissues, cartilage and bone for orthopedic applications. Additionally, it is personally gratifying to be able to support the SCRMC while my son completes his senior year studying neurobiology at UW–Madison. We are happy to be part of the University of Wisconsin family."
Li shared that the donation was profoundly impactful and allowed him to further his goal of using stem cells to help patients struggling with osteoarthritis as well as other joint diseases.
"I want to make sure that our findings in stem cell research can be used to help people," says Li. "I just feel this internal drive to study this area and I feel good knowing this model carries significant weight in terms of its potential for translational stem cell research and the development of therapeutic treatments."
This research was supported by grants from the National Institutes of Health (R01 AR064803) and the Plunkett Family Foundation. The UW Department of Pathology and Laboratory Medicine and UWCCC (P30 CA014520) and the Small Animal Imaging and Radiotherapy Facility and Flow Cytometry Laboratory, supported by UWCCC (P30 CA014520) also provided facilities and services.
Source: University of Wisconsin-Madison, which is solely responsible for the information provided, and wholly owns the information. Informa Business Media and all its subsidiaries are not responsible for any of the content contained in this information asset.
You May Also Like



